While the flexible nature of modular medial units allows for a robust and comprehensive array of medical spaces and functions, the benefits do not stop there. No matter if the modules are deployed to assist after a natural disaster or to accommodate temporary overflow at a rural hospital, the customizable framework offers wide-ranging value.
Increased Speed to Market
In contrast with the standard design and construction approach of a brick-and-mortar facility on a hospital or healthcare system campus, modular medical units work within the distinct structural base of an ISO shipping container. While the modules can be configured in unique and flexible ways, the definitive aspects of the base allow for shortened processes around deployment.
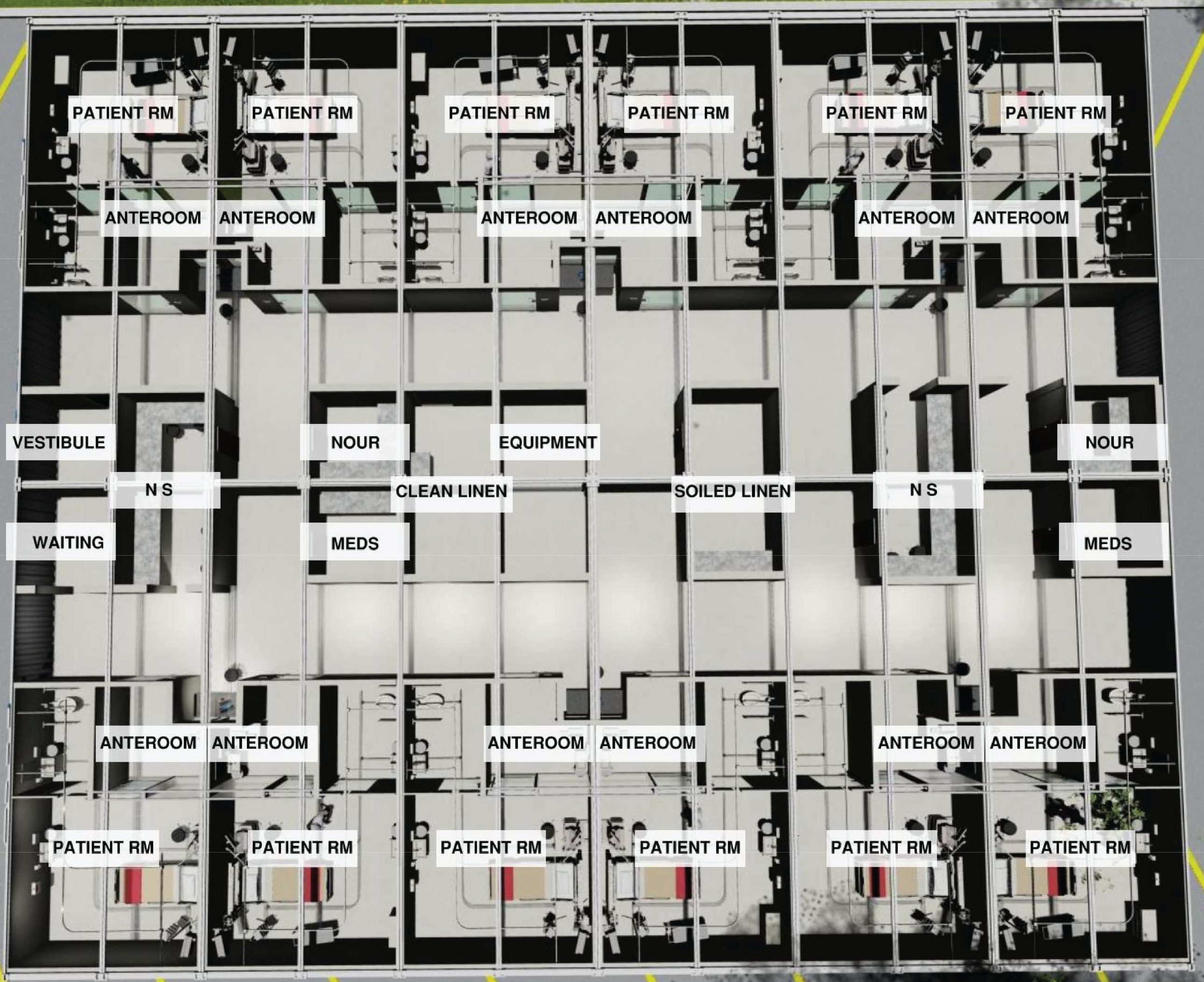
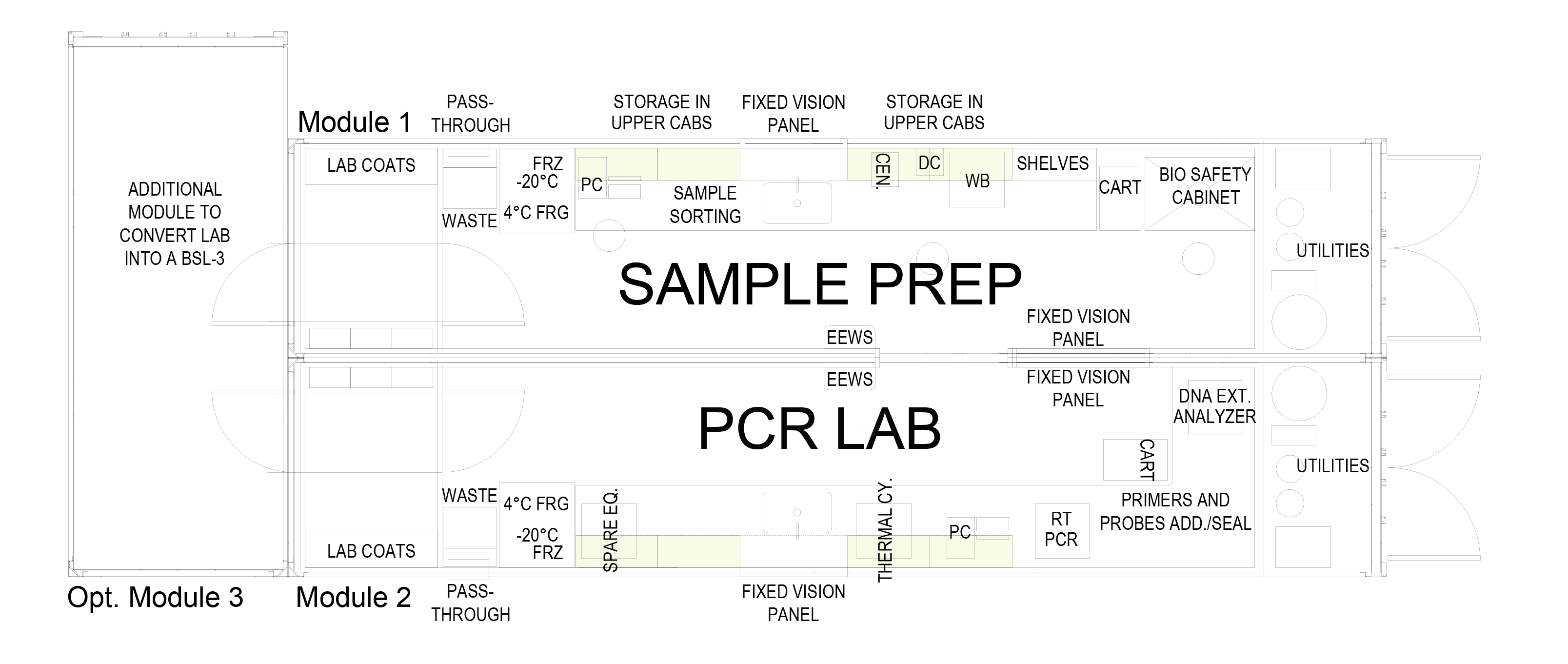
For one, the fixed framework, prefabrication and known square footage of the containers abbreviate design timelines from those starting with a blank slate. For example, a project for an eight-bed ICU would begin with an understanding that 20 to 25 modules would be needed to achieve the needed square footage. From there, the hospital or healthcare system would be able to view a standard layout for its need within the structured framework and begin customizing to its specifications.
From there the design would be sent directly to a prefabrication shop to build the customized modules. Prefabrication itself is a truncated method for traditional construction, because so much of the work is completed off-site in a controlled environment. Prefabrication boasts an efficient process of precutting materials and assembling sections within streamlined workflows to reduce hours on an active healthcare campus. The off-site nature of prefabrication also eliminates pauses for weather events and potentially limited craft labor resources, helping to reduce delays.
Once all the modules are fabricated and precommissioned, they are transported and assembled on-site. This process would involve physically interlocking the many modules, establishing the environment for immediate use, and commissioning the final product based on strict healthcare standards. In stark contrast with a traditional brick-and-mortar facility, this assembly approach can turn months or even years of disruptive on-site construction into weeks.
A Quality Construction Solution
In addition to saving time, the tried-and-true method of prefabrication for modular medical units allows the essential elements and core requirements to be built in a controlled indoor environment. This provides not only safer work conditions — by eliminating the need to build pieces on-site, often at great heights or in potentially hazardous outdoor conditions — but also consistency in workforce.
Within prefabrication facilities, specialized workers can concentrate on a linear production process when creating components while adhering to frequent checks and balances. This repetitive, concentrated process from dedicated craft laborers results in high-quality module output.
Prefabrication also allows all construction — aside from site assembly — to be removed from crowded, fully operational healthcare campuses or potentially hazardous surroundings after a natural disaster. Therefore, the modules are fully completed, checked and approved, including all headwalls, medical gas outlets, exam lights and medical gas booms, before they are loaded for transport.
Reduced Capital Budget Strain
With such flexibility in medical use case and configuration, modular medical units also provide flexibility to capital budget expenditures and resources. By accommodating temporary and permanent deployments, hospitals and healthcare systems can determine the right approach for both their short- and long-term goals.
For example, a hospital may not have laboratory capacity to handle the pandemic testing surge or isolation bed overflow. However, though meeting the immediate need is essential, a brand new brick-and-mortar facility may not be appropriate in the long term. Therefore, a temporary modular medical unit configured for a lab and 12-bed isolation patient rooms could allow the hospital to provide necessary care without dipping into the capital costs of hard construction.
On the other hand, an emergency room is a long-term asset that a rural hospital location may need to serve its communities. If capital isn’t available for a brick-and-mortar addition, or if labor costs are too high in the area, a free-standing modular configuration could provide that long-term service with a relatively short recovery of the investment.