One major health insurance system sought to implement an entirely new concierge primary care model. This case was a rare opportunity, and not every organization has the opportunity to start from scratch in designing a new patient experience. The fundamental takeaways from this engagement, however, are applicable to projects of any size, including both new facilities and remodels.
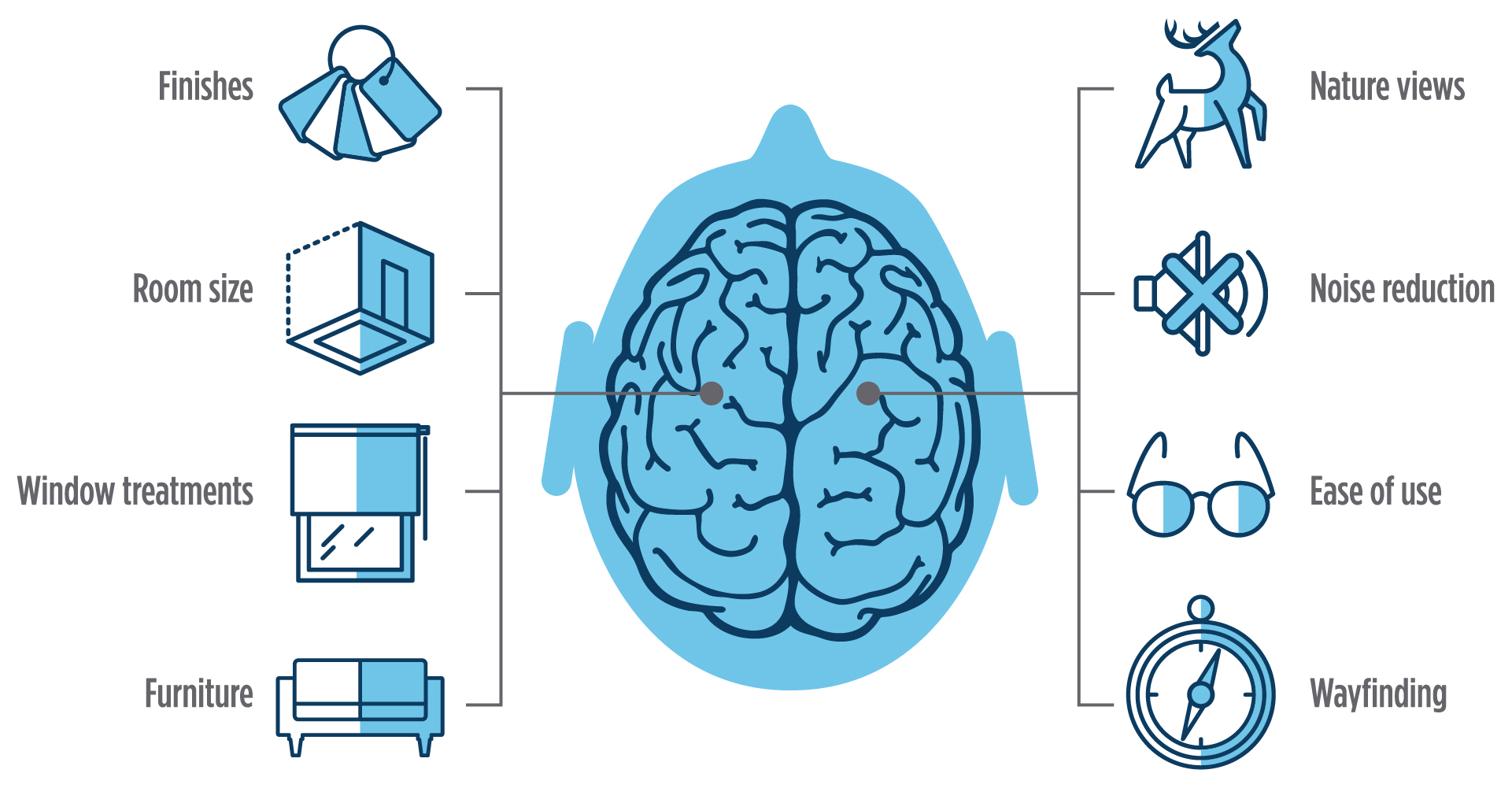
The project began with a focused research project designed to help understand what customers wanted from their health insurance plan. This initial research, drawing on behavioral studies, focus groups and other research, reached an interesting conclusion: People wanted a place to engage with their healthcare concerns, not just an insurance plan. Less than two years later, this research drove the creation of the health plan’s first care center, based on a design directly informed by customers’ feedback. For example:
- Customers wanted to complete requisite paperwork ahead of time. Procedures were adjusted to see that all paperwork was electronically available to patients in advance of visits. This change helped reduce waiting times, gave patients time to gather all the needed information and reduced stress upon arrival for their visit. Based on a series of dedicated design sprints, the system implemented strategic member experiences for pre-arrival, greeting and post-visit wraparound services like behavioral health services and health coaching.
- Patients wanted their healthcare provider to know them individually and anticipate their arrival. With paperwork completed ahead of time, front desks could be redesigned to focus less on gathering information and more on providing a welcoming experience. Front desks were designed as high-top, solid surfaces, easily approachable and located immediately by the front door. To focus this space on human interaction, these welcome desks would feature no phones or computer monitors. Any necessary sign-in procedures would be performed by staff via iPad.
- In exam rooms, local art and comfortable furniture gave rooms the feel of a home living room, with monitors that could provide education, and other visible equipment minimized.
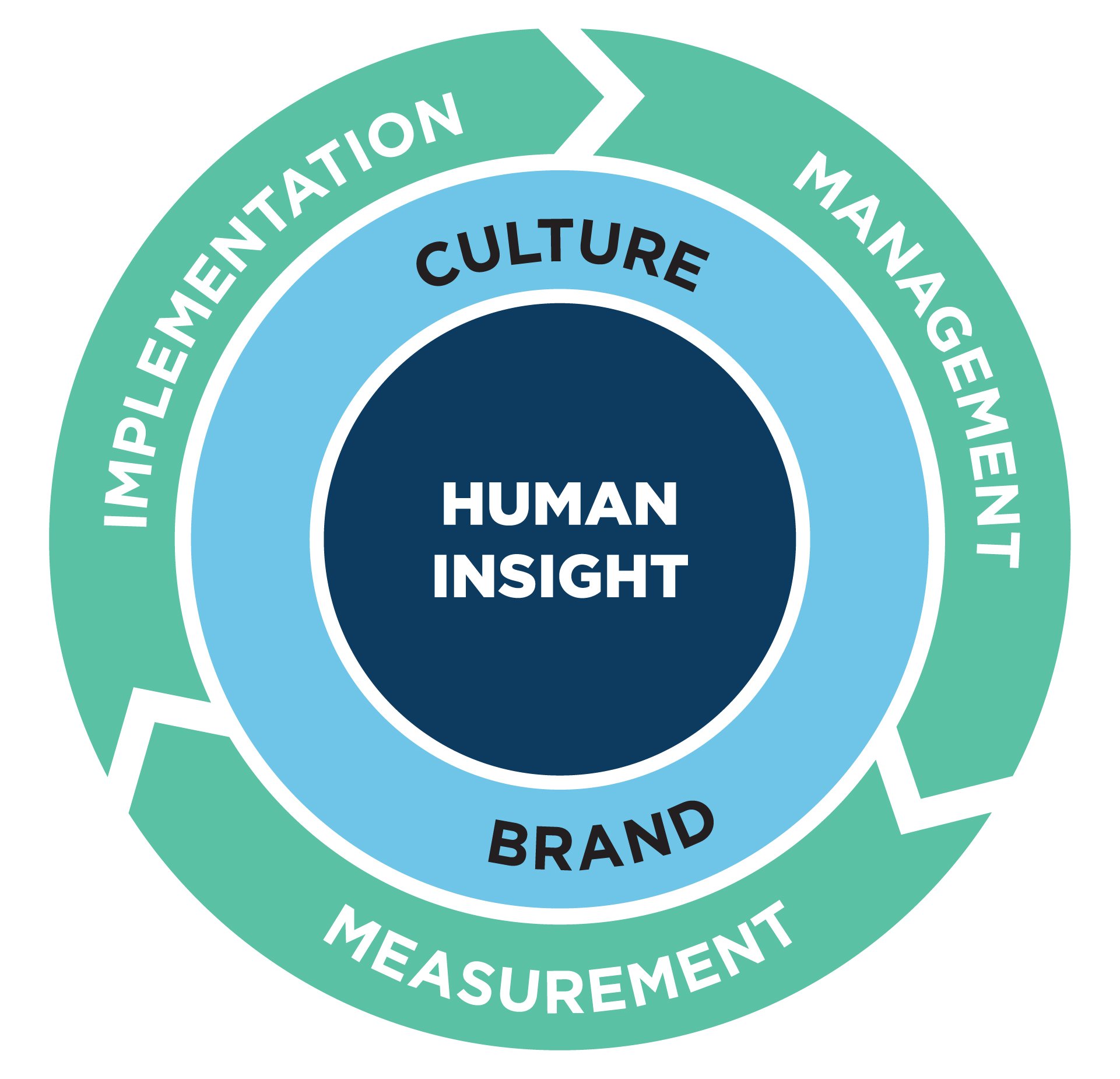
The system defined hiring processes designed to emphasize empathy, part of a systematic effort to develop a culture built on a human-centered patient experience. These efforts extended to the brand itself, which shifted terminology to focus on care (employing care centers, care guides and care advocates) and to emphasize membership in the plan as something underpinned by a real sense of trust, support and belonging. Patients were referred to as members.
Moving forward, improvement would be measured using care team surveys, member surveys (with items specifically tailored to reflect the type of visit) and patient input from a real-time experience rating tool. After one year, the leadership team conducted a three-day listening tour to gather input and create a detailed action plan for continuous improvement in the program’s second year. During new member orientation, members would meet with a care guide at the conclusion of the visit, an opportunity to collect more detailed qualitative feedback on the experience. Open houses for prospective members were also leveraged as an opportunity to collect further feedback on the desired patient experience. As this feedback was received, the design and facilities team, operational and clinical leadership, and original research partner came together to utilize these new insights to make changes to the overall layout and offerings at future care centers.